
Mechanical thrombectomy after stroke has significantly improved prognosis in some clinical situations. However, information on indications in guidelines is scarce or unclear. So there are many different situations where clinical decisions need to be made based on very weak evidence.
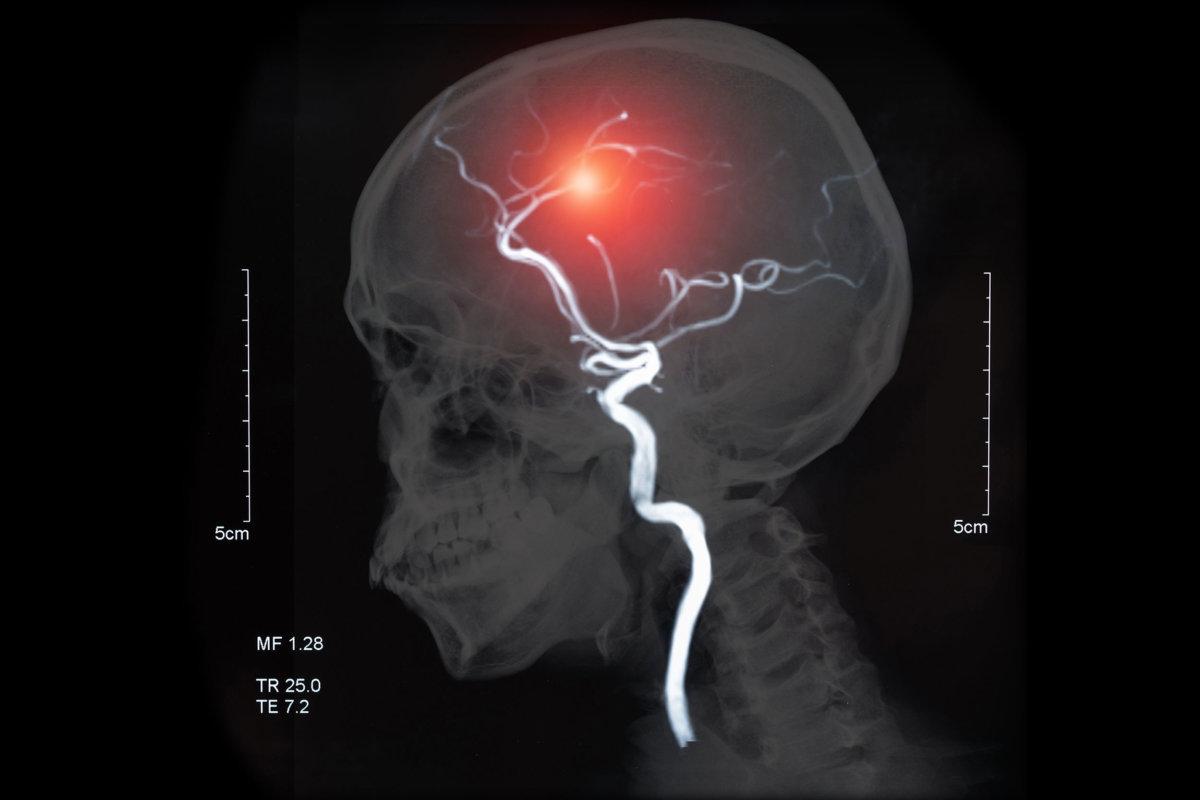
utah51/AdobeStock
The German S2 guideline for the management of acute stroke, in which the Austrian and Swiss expert societies are also involved, states that mechanical thrombectomy is indicated in “patients with severe ischemic stroke, clinically relevant neurological deficits and occlusion of the great anterior circulation”. , no more than 6 hours between onset of symptoms and lumbar puncture. This very short time window can be extended to 24 or more hours in some circumstances. Patients in good pre-existing health are eligible for this treatment if they have an NIHSS (National Institutes of Health Stroke Scale) score of at least 6 and an ASPECTS (Alberta Stroke Program Early CT Score) of 6. However, the guideline also states that endovascular therapy “may also be useful in patients who do not fit these criteria.”
This means that there are numerous situations in everyday clinical practice where the indication for revascularization using thrombectomy is by no means trivial, says Professor Dr. Patrick Michel, University of Lausanne. In Switzerland, the criteria for thrombectomy and intravenous thrombolysis are a premorbid score of at least 3 on the Rankin scale (corresponding to moderate impairment), a life expectancy of at least 3 months with an acceptable quality of life and an NIHSS score of at least 4 and/or impairment leading to disability. In Michael's center, another criterion is the main zone of cardiac infarction, which should not exceed three quarters of the entire ischemic area. Michael: “It keeps us from doing stupid things.”